Why pain appears in your 40s!
Many women I see in their 40s and 50s start conversations with something like this:
“I don’t understand what’s going on. I’ve always been active, I look after myself… and yet my body just doesn’t feel the same.”
The pain isn’t dramatic. There’s no obvious injury. It’s more of a background issue - a stiff hip that doesn’t quite settle, a back that feels more vulnerable, pelvic discomfort that comes and goes.
It’s unsettling, and often quietly frustrating.
If this feels familiar, you’re certainly not alone.
This isn’t “just ageing”
One of the most important things I want women to hear is this: pain appearing in your 40s does not automatically mean your body is deteriorating.
For many women, this stage of life brings subtle but meaningful changes in how the body responds to everyday demands. Hormonal shifts associated with peri-menopause can influence connective tissue, muscle tone and joint stiffness. Recovery after exercise may take longer than it once did. Sleep is often lighter or more disrupted, which affects how well tissues repair and how the nervous system processes pain.
Add in the background load of work, family, caring roles and ongoing stress, and it’s easy to see why the body can start to feel less forgiving - even when nothing is “wrong”.
Why pain can appear even when you’re doing everything right
This is often the most confusing part. Women tell me they haven’t changed what they do - they’re still walking, running, doing Pilates or yoga - but their body seems to be responding differently.
What’s usually happening is that the body’s tolerance for load has shifted slightly. Things it once absorbed easily now need a bit more support, better recovery, or a small adjustment in how they’re done.
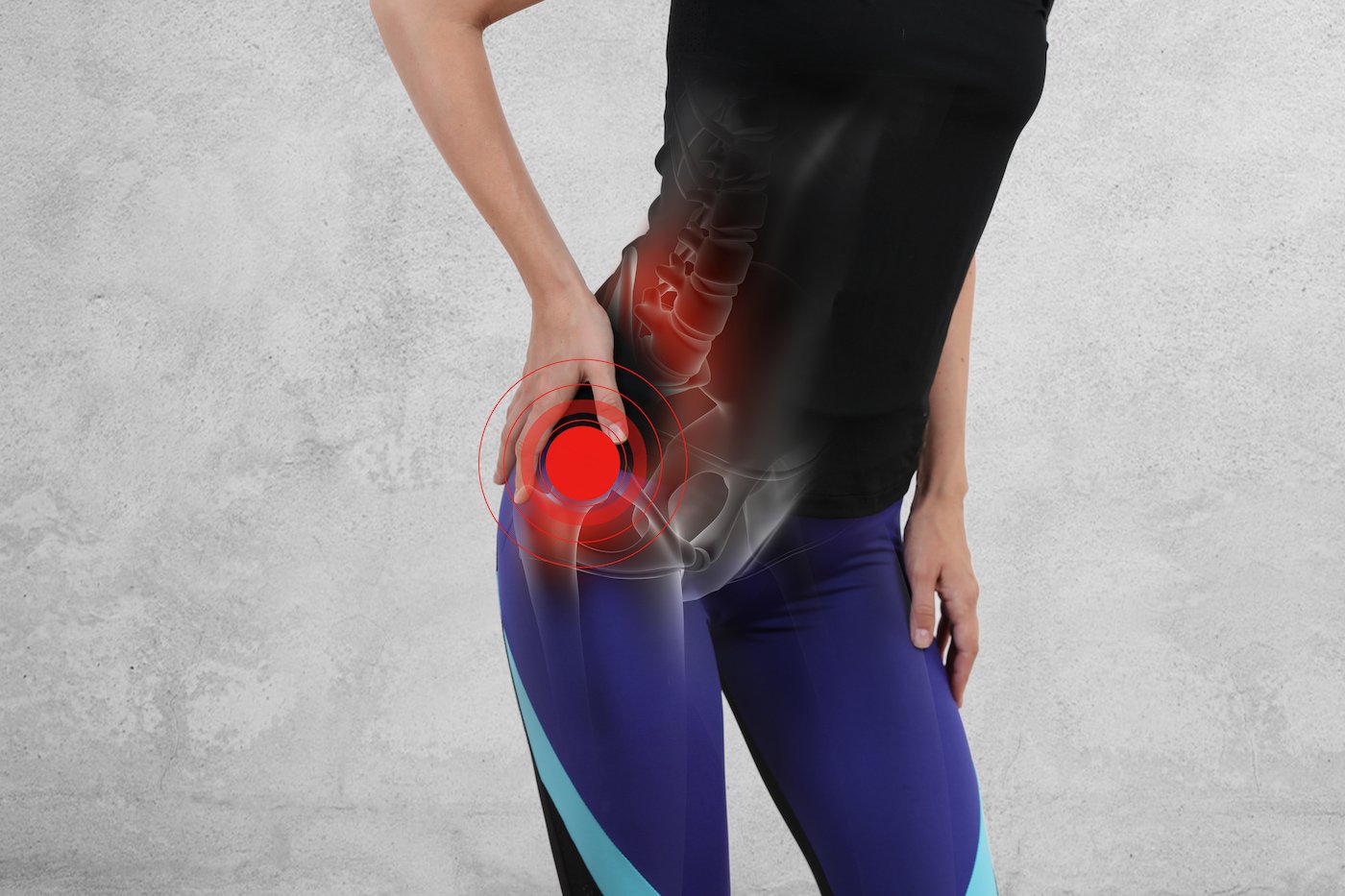
This is particularly common around:
the hips
the pelvis
the lower back
the pelvic floor
If sleep is poor, stress levels are high, or nutrition isn’t quite supporting recovery, the body has less capacity to adapt. Pain, in this context, is often a sign that something needs adjusting - not that something is damaged.
Why scans are often normal
Though reassuring, “normal” scans can also be puzzling or frustrating. Women can feel confused and demoralised, even leading to psychological distress.
Imaging is excellent at identifying serious pathology. What it doesn’t show particularly well are things like muscle tension, joint stiffness, movement patterns, breathing mechanics, or how sensitised the nervous system might be.
Pain is influenced by far more than structure alone. Stress, fatigue, poor sleep and ongoing low-level inflammation can all amplify symptoms without leaving a trace on a scan. So a normal result doesn’t mean nothing is going on - it simply means the problem isn’t something imaging can capture.
The good news
The body in midlife is not fragile. In fact, it often responds extremely well once the right factors are addressed.
For many women, improvement doesn’t come from doing more, but from doing things differently. There are several modifiable factors that can significantly influence how pain behaves.
Movement remains important, but the focus often shifts from pushing through discomfort to supporting strength, mobility and recovery. This might mean adapting how you exercise, spacing sessions out more thoughtfully, or choosing movement that builds resilience rather than constantly challenging your limits.
Stress plays a larger role than many women realise. When the nervous system is under constant pressure, muscles tend to hold more tension and pain is more likely to linger. Learning how, and when, to genuinely slow down can have a surprisingly positive effect on symptoms.
Sleep is one of the most powerful tools for pain regulation. Poor or disrupted sleep reduces the body’s ability to repair tissue and modulate pain. Even small improvements in sleep quality can change how the body feels day to day.
Nutrition also matters. Stable blood sugar, adequate protein, and sufficient nutrients all support tissue health and recovery. This isn’t about restrictive diets or perfection, it’s about giving the body enough fuel to cope with what’s being asked of it.
When these factors are addressed alongside hands-on treatment and a clear understanding of what’s driving the pain, the body often settles far more readily than women expect.
When to seek help
It’s worth having things properly assessed if pain is:
lingering rather than easing
affecting sleep
reducing enjoyment of activity
flaring when you’re stressed, tired or unwell
coming and going without a clear pattern
In my clinic between Farnham and Odiham, I often see women who’ve been quietly putting up with symptoms for months or even years — assuming it’s just part of getting older.
It rarely is.
Sometimes, a small shift in understanding and treatment makes a surprisingly big difference!